MBRRACE-UK perinatal mortality surveillance
Technical manual
Version 1.4.
Contents
1. MBRRACE-UK methods for reporting perinatal mortality rates
1.1. Deaths reported to MBRRACE-UK
Deaths reported to MBRRACE-UK since 1 January 2013 are:
- Late fetal losses – the baby is born at 22 or 23 completed weeks’ gestation showing no signs of life, irrespective of when the death occurred.
- Stillbirths – the baby is born from 24 completed weeks’ gestation (or from 400g where an accurate estimate of gestation is not available) showing no signs of life, irrespective of when the death occurred.
- Neonatal deaths – the death of a live born baby born from 20 completed weeks’ gestation (or from 400g where an accurate estimate of gestation is not available) occurring before 28 completed days after birth.
Terminations of pregnancy resulting in a registered stillbirth (from 24 completed weeks’ gestation) or neonatal death (from 20 completed weeks’ gestation) are also notified. We collect this limited information about terminations of pregnancy in order to exclude these cases from MBRRACE-UK reported statistics on perinatal mortality.
In an effort to ensure complete data collection and to facilitate international comparisons, the eligibility criteria for MBRRACE-UK are based on gestational age at delivery irrespective of when the death occurred. Therefore, all births delivered from 22 completed weeks’ gestational age showing no signs of life must be reported, irrespective of when the death occurred; the date of delivery and date of confirmation of death are both reported for these deaths. For all deaths, where an accurate estimate of gestation is not available a minimum birthweight of 400g is used to determine eligibility. For multiple pregnancies, where there is more likely to be a longer gap between an in utero death and the subsequent birth, deaths are excluded where the death is confirmed before 20 completed weeks' gestational age.
MBRRACE-UK operates a secure online reporting system which can be accessed by all UK Trusts and Health Boards providing maternity and neonatal care. Responsibility for reporting a death and for the completeness and the quality of the data reported to MBRRACE-UK lies with the Trust or Health Board where the death occurred. Each Trust and Health Board has identified a small number of MBRRACE-UK Lead Reporters who act as key points of contact between their organisation and MBRRACE-UK. In order to check for any relevant deaths that have not been reported to MBRRACE-UK, details of statutorily registered deaths are obtained from the Office for National Statistics (ONS) (England and Wales), National Records of Scotland (NRS) (Scotland), Northern Ireland Maternity System (NIMATS) and Northern Ireland Statistics and Research Agency (NISRA) (Northern Ireland), Health and Social Services Department (Bailiwick of Guernsey), and Health Intelligence Unit (Bailiwick of Jersey). More details of the MBRRACE-UK reporting system are given in Section 3.
1.2. Information collected by MBRRACE-UK
Comprehensive information about each death is requested by MBRRACE-UK in order to allow detailed examination of the risk factors for perinatal mortality in the UK. Data items are collected with the aims of, first, offering more appropriate adjustment of the crude mortality rates than had previously been possible and, second, providing a clearer insight into the health, social and lifestyle factors most commonly associated with stillbirth or neonatal death. The data relating to each death consists of information about the following:
- mother’s and baby’s identifying information (to permit the cross-checking of each death against other national databases and to facilitate the identification of duplicate records);
- mother’s health, lifestyle and previous pregnancy history;
- mother’s antenatal care;
- labour and delivery;
- cause of death and post-mortem examination.
Details of the data requested for each late fetal loss, stillbirth and neonatal death can be found in Section 4. Approvals have been obtained from all relevant authorities in order for identifiable data to be collected without consent and to access statutory birth and death information (Section 3).
1.3. The birth cohort
Rates of stillbirth, neonatal death and extended perinatal death are presented for births from 1 January to 31 December in the reference year; thus, neonatal deaths of babies born in December 2021 which occurred in January 2022 are included in the report for 2021 births. The reporting of mortality for a birth cohort is in contrast to statutory publications, which are based on deaths in a calendar year. This method of reporting allows more accurate estimates of mortality rates to be produced, as appropriate denominators are available.
Individual level information on all births in the UK and Crown Dependencies is obtained in order to generate mortality rates adjusted for maternal, baby, and socio-demographic risk factors. Information for England, Wales and the Isle of Man (Personal Demographics Service (PDS) and ONS birth registration data), Scotland (NRS and Public Health Scotland; PHS), Northern Ireland (NIMATS), Bailiwick of Guernsey (Health and Social Services Department) and the Bailiwick of Jersey (Health Intelligence Unit) are combined to give a single dataset of births for the whole UK and Crown Dependencies. This data is then combined with the information on the deaths to obtain the final data for analysis. Details of the generation of the births dataset are provided in Section 3.
1.4. Deaths included in reported mortality rates
In order to facilitate the comparability of mortality rates between organisations, and unless stated otherwise, births less than 24 completed weeks’ gestational age and terminations of pregnancy are excluded from the mortality rates reported. This avoids the influence of the wide disparity in the classification of babies born before 24 completed weeks’ gestational age as a neonatal death or a fetal loss, as well as the known variation in the rate of termination of pregnancy for congenital anomaly across the UK. The mortality rates reported include all eligible deaths, including deaths due to congenital anomalies, unless stated otherwise.
The number of deaths of babies born in the UK in the reference year as described by MBRRACE-UK will differ from that of statutorily registered deaths published by ONS (England and Wales), NRS (Scotland) and NISRA (Northern Ireland) because of the exclusion criteria used in this report to ensure standardisation of mortality rates. It is important to recognise that data sources from statutorily registered births and deaths include both birth and death registrations following termination of pregnancy from 24 completed weeks’ gestational age and variable inclusion of births at 23 completed weeks’ gestational age and below, depending on whether they were reported as being liveborn or not. MBRRACE-UK receives stillbirth and neonatal death registrations from statutory sources. This data is matched to the detailed MBRRACE-UK death notifications. Of these registered deaths, neonatal deaths are excluded if delivery was before 24 completed weeks’ gestational age or they were a termination of pregnancy (deaths are classified as resulting from a termination of pregnancy based on the detailed MBRRACE-UK data).
In addition to registered deaths obtained from ONS, NRS and NISRA, additional deaths are reported to MBRRACE-UK for:
- the small number of deaths statutorily registered with ONS, NRS or NISRA only after considerable delay, most often because an inquest was being held;
- late fetal losses delivered at 22 to 23 completed weeks’ gestational age which are not subject to statutory registration;
- stillbirths delivered at 24 completed weeks’ gestational age or greater where the death was confirmed before 24 completed weeks’ gestational age; these are not routinely registered as stillbirths, as recommended by RCOG guidance and agreed with the Department of Health.
1.5. Organisations for which mortality rates are reported
Rates of stillbirth, neonatal death, and extended perinatal death are reported for four groups of clinical and administrative organisations:
-
Organisations responsible for population-based care commissioning based on postcode of mother’s residence at time of delivery:
- England: Integrated Care Boards (ICBs); sub-Integrated Care Board Locations (sub-ICBs);
- Scotland: National and Health Boards;
- Wales: National and Health Boards;
- Northern Ireland: National and Local Commissioning Groups;
- Crown Dependencies: Isle of Man, Bailiwick of Guernsey, and Bailiwick of Jersey.
-
Service delivery organisations based on place of birth:
- England: NHS Trusts;
- Scotland: Health Boards;
- Wales: Health Boards;
- Northern Ireland: Health and Social Care Trusts;
- Crown Dependencies: Isle of Man, Bailiwick of Guernsey (until 2022), and Bailiwick of Jersey.
-
UK Neonatal Networks based on place of birth.
-
Local government areas based on postcode of mother’s residence at time of delivery:
- England: Single tier authorities, upper tier authorities and London boroughs;
- Scotland: Unitary authorities;
- Wales: Local authorities;
- Northern Ireland: Local government districts;
- Crown Dependencies: Isle of Man, Bailiwick of Guernsey (until 2022), and Bailiwick of Jersey.
1.6. Analysis of mortality rates
Three mortality outcomes are reported for each organisation: stillbirth, neonatal death, and extended perinatal death. These mortality rates are presented in a number of different ways, depending on organisation type: as a ‘crude’ mortality rate, a ‘stabilised’ mortality rate and a ‘stabilised & adjusted’ mortality rate.
The crude mortality rate is the number of deaths divided by the number of total births (or live births in the case of neonatal mortality) for the reported year and provides an annual snapshot of the mortality in an organisation.
While the crude rate is informative, in that it describes exactly what happened for the organisation, it can be potentially misleading when trying to highlight organisations where the mortality rate is higher than expected due to variation in the quality of care. The number of perinatal deaths for many organisations is likely to be small, as these deaths are rare, and there will be more deaths in some years than in others just by chance. This can lead to large fluctuations in the annual crude mortality rate, especially for organisations that have a very small number of births.
In order to compare organisations more fairly, mortality rates are stabilised. Where there is only a small number of births in an organisation it is difficult in any one year to be sure that any extreme value seen for the crude mortality rate is real and not just a chance finding. A stabilised rate allows for the effects of chance variation due to small numbers. For this reason, the stabilised mortality rate will tend to be closer to the average mortality rate than will the crude mortality rate, especially for organisations with a small number of births. For mortality rates based on the mother's residence (organisations commissioning care or carrying out public health initiatives to reduce perinatal mortality, such as Integrated Care Boards or Local Authorities), crude and stabilised mortality rates are presented followed by a table detailing the risk factor profiles for each population to facilitate the development and targeting of interventions.
For service delivery organisations, some organisations have a higher proportion than others of women at high risk of experiencing a stillbirth or neonatal death: for example, they provide a national or regional specialist service or serve areas of high socio-economic deprivation. Thus the case-mix of the service users can influence mortality rates even when high quality maternity and neonatal care is provided. The mortality rates based on place of birth (service delivery organisations, such as Trusts and Health Boards, or Neonatal Networks) are, therefore, also adjusted to account for key factors which are known to increase the risk of perinatal mortality: i.e. stabilised & adjusted mortality rates. The extent of the adjustment is limited to those factors that are collected for all births across the whole of the UK: mother’s age; socio-economic deprivation based on the mother’s residence; baby’s ethnicity; baby’s sex; whether they are from a multiple birth; and gestational age at birth (neonatal deaths only). Therefore, some factors that might be associated with poor perinatal outcomes could not be taken into account in the adjustment because they are not universally collected on all births; for example, maternal smoking and body mass index (BMI). As for stabilised rates, the stabilised & adjusted mortality rate will also tend to be closer to the average mortality rate than will the crude mortality rate, especially for organisations with a small number of births.
It is important to remember that the mortality rates reported are not definitive measures of the quality of care received by any individual or group. Some of the variation in mortality rates shown in the report might be the result of differences in the proportion of high-risk pregnancies that cannot be accounted for in the analyses due to a lack of routinely collected detailed clinical information for all births (as described above). However, given the information that is available, the rates reported by MBRRACE-UK are robust and make an important contribution in highlighting those organisations where extra investigations should be targeted in order to improve the quality of perinatal and neonatal care in the UK.
1.7. Identifying potentially high and low rates of death
The crude, stabilised and stabilised & adjusted mortality rates are presented as both tables and maps. In the maps, each organisation is colour coded based on the extent to which their particular mortality rate is above or below the ‘average’ mortality rate. For the organisations based on the postcodes of the mothers’ residences at time of delivery, and for Neonatal Networks, this average is the overall observed mortality rate for the whole of the UK and the Crown Dependencies.
However, it is known that service delivery organisations based on the place of birth vary widely in the risk profile of pregnancies referred to their service; therefore, it is reasonable to anticipate variation in their expected mortality rates. To help account for the variation due to the risk profile, all Trusts and Health Boards are classified hierarchically into five mutually exclusive comparator groups based on their level of service provision and are compared to the average mortality rate within their comparator group. The five comparator groups are:
- Level 3 Neonatal Intensive Care Unit (NICU) and neonatal surgery;
- Level 3 NICU;
- 4,000 or more births per annum at 22 weeks or later (no level 3 NICU);
- 2,000-3,999 births per annum at 22 weeks or later (no level 3 NICU);
- Under 2,000 births per annum at 22 weeks or later (no level 3 NICU).
Organisations are then categorised according to whether their mortality rates are above, similar to or below the average rates for organisations providing similar levels of care. We use colour coding to represent mortality rates in the data viewer and in the reports issued to Trusts and Health Boards.
The colour coding is as follows:
- Green: more than 15% lower than the average.
- Yellow: more than 5% and up to 15% lower than the average.
- Amber: up to 5% higher or up to 5% lower than the average.
- Red: more than 5% higher than the average.
Within the data viewer, the size of the circles on each map represents the number of births in the population covered by the particular organisation, although there is a minimum size in order that the colour can be adequately seen.
The accompanying tables show either both the crude and the stabilised rate for stillbirth, neonatal death, and extended perinatal death or the crude and the stabilised & adjusted rate for stillbirth, neonatal death, and extended perinatal death for each organisation, as appropriate.
1.8. Suppression of rates calculated when there are few deaths
In order to avoid disclosure of information which could potentially identify individuals, crude mortality rates based on a very small number of deaths are not included, in line with guidance from ONS and the Government Statistical Service. Suppressed mortality rates are shown as a white dot on the maps and as -1 in the tables, where appropriate.
1.9. Classifying cause of death
Causes of death are reported to MBRRACE-UK using the Cause of Death & Associated Conditions (CODAC) classification system. The CODAC system has a three-level hierarchical tree for the coding of both the primary cause of death and any associated conditions. The CODAC level 1 and level 2 classification is presented for all stillbirths and neonatal deaths.
When reporting a death via the MBRRACE-UK data entry system reporters are asked to complete both a primary cause of death and up to two associated conditions. Following a detailed review of the coding of deaths reported as due to congenital anomalies in the 2015 MBRRACE-UK report, all cause of death data is presented using congenital anomaly as the cause of death for all deaths where a congenital anomaly is coded as either the primary cause or an associated condition
2. Statistical methods
2.1 Calculation of stabilised & adjusted mortality rates
The stabilised & adjusted mortality rate for each organisation (mj) is calculated by multiplying the appropriate 'comparator' mortality rate (M) by an organisation-specific standardised mortality ratio (SMRj) calculated from the data, i.e.:
where
mj is the estimated stabilised & adjusted mortality rate for organisation j
M is the appropriate comparator mortality rate
SMRj is the estimated SMR for organisation j:
Currently, for all organisations, except for the Trusts and Health Boards of birth, the comparator mortality rate is the overall mortality rate for the whole of the UK and Crown Dependencies. For the Trusts and Health Boards of birth the comparator mortality rate is the overall rate for Trusts and Health Boards in the same comparator group (described below).
The SMR is estimated using a multilevel logistic regression model. A multilevel model is used as it can accommodate the hierarchical structure of the data through the random term; that is, births clustered within organisations. These models also allow the calculation of stabilised (also known as ‘shrunken’ or ‘smoothed’) estimates of the organisation-specific terms, which reduce the likelihood of organisations being falsely identified as outliers by chance alone.
Various approaches to calculating a SMR from a multilevel logistic model have been proposed. The method used for the MBRRACE-UK report “… is determined by dividing the smoothed, risk-adjusted, provider-specific estimate of mortality by the estimate of expected mortality obtained using the average intercept for all … providers”. In this approach, the observed number of deaths is replaced by a model-based predicted number reflecting sampling variation in the observed deaths; that is, a stabilised observed number of deaths is estimated for each organisation. Hence, the SMR is the ratio of the stabilised number of deaths to the deaths that would be expected if the organisation’s patients were from an ‘average’ organisation.
2.2. Statistical models
Two multilevel logistic regression models are used, one for the stillbirths as outcome and the other model for neonatal deaths. The reference group for the both models is the births surviving at least 28 days from birth. The multilevel logistic regression model for stillbirth compared to survival to the end of the neonatal period is:
where
Y(SB)ij is the indicator variable of stillbirth for the ith baby in the jth organisation:
Y(SB)ij = 1 if stillbirth; 0 if survivor to end of neonatal period; missing if neonatal death;
xij is the vector of risk-adjustment factors for the ith baby in the jth organisation
zij is the vector of risk-adjustment factors for the jth organisation
δ(SB)j is the random term representing organisation j: δ ~ Normal(0,σ2)
A similar model is estimated for neonatal deaths compared to survival to the end of the neonatal period:
where
Y(NND)ij is the indicator variable of neonatal death for the ith baby in the jth organisation:
Y(NND)ij = 1 if neonatal death; 0 if survivor to end of neonatal period; missing if stillbirth;
xij is the vector of risk-adjustment factors for the ith baby in the jth organisation
zij is the vector of risk-adjustment factors for the jth organisation
δ(NND)j is the random term representing organisation j: δ ~ Normal(0,σ2)
The SMR for stillbirth is then given by combining these two models:
The SMR for neonatal deaths is derived directly from the second multilevel logistic regression model, since stillbirths are not included in the calculation of neonatal death rates:
3. Further details of MBRRACE-UK data collection
3.1 Approvals for collection of patient identifiable data
The necessary approvals obtained by the MNI-CORP programme prior to the start of the data collection process are listed below. These are applied for in order to collect patient identifiable data and access information collected by statutory organisations without consent.
England and Wales
- The Confidentiality Advisory Group of the Health Research Authority: ECC 5-05 (f)/2012 (from 10 October 2012); 15/CAG/0119 (from 1 May 2015)
- Health & Social Care Information Centre, Data Access Advisory Group: IC604DS
Scotland
- The NHS Scotland Caldicott Guardian: 2014-62 MBRRACE-UK Programme – Update (2013-05)
- The Privacy Advisory Committee, ISD, NHS National Services Scotland: PAC16/14
Northern Ireland
Due to the different data privacy arrangements in Northern Ireland, only de-identified data is provided to the MNI-CORP programme. This data is supplied by the NIMACH office.
3.2. The system for online data submission
Security
Access to the MBRRACE-UK website is via the internet using the secure HTTPS protocol. The web and database servers are housed in a secure data centre with firewall protection. All staff requesting online access must be approved by their Trust or Health Board and log-in is only possible with either an NHS or UK university email address. When an approved reporter first accesses the website they are required to request an activation code. This is used as a one-time password which must be changed on first access. All passwords must meet a set of criteria which ensures all passwords accepted are ‘strong’. Reporters are assigned a profile which restricts their access to only the appropriate parts of the website for their role (the system is used to report deaths, to review deaths with the Perinatal Mortality Review Tool (PMRT), and to provide access to anonymised medical case notes for assessors taking part in MBRRACE-UK confidential enquiries).
All patient identifiers are encrypted before they are stored. Access to identifiable data is only allowed under very limited circumstances. Reporters may view the data from their own Trust or Health Board (subject to the use of a valid password) while access to identifiable data by MBRRACE-UK staff is subject to NHS information governance, security and confidentiality regulation.
Data integrity and validation
Reporters wishing to report a new death or edit an existing death record are required to confirm the mother’s details (NHS or CHI number, name, date of birth) on each occasion. The nationally defined algorithm for checking NHS and CHI numbers is used to ensure only valid numbers are entered.
Where appropriate, the information reported is checked against a range of acceptable values during the data entry process. For each such data item there is a range of expected values and an absolute range. If a value is outside the expected range the reporter is warned and informed of the range. If it is outside the absolute range then the value cannot be entered and, additionally, the record cannot be closed. Before the reporter can close a record additional checks are carried out; for example, date values across the whole record are validated against each other to test for consistency.
In some circumstances there may be a small number of data items that are unavailable. In these situations reporters may indicate that an item is ‘not known’, with an opportunity to add the missing data at a later date.
For a significant number of deaths some of the data required will be held in more than one hospital, e.g. some aspects of maternal data after the death of a baby following postnatal transfer. If the additional information is held within the same Trust or Health Board but on a different site then reporters can access all the information they need in collaboration with obstetric, midwifery, neonatal or nursing colleagues. However, if the missing information is held by a different Trust or Health Board, then the MBRRACE-UK system allows the reporter to temporarily assign ownership of the MBRRACE-UK record to the other Trust or Health Board who can then return it once the missing information has been provided.
Online help
On every data entry screen many of the variables have specific help available by clicking on the ‘Help’ icon. Also, on every screen of the website there is a function to allow the reporter to enter a help request. This is sent via email to the MBRRACE-UK office for attention by the technical, clinical or administrative staff, as appropriate. A detailed user manual is also available to download from the MBRRACE-UK system.
Reports
The MBRRACE-UK online reporting system allows reporters access to information relating to local deaths:
- the Trust/Health Board Case Summary list provides abbreviated details of all deaths reported in an individual birth year together with the current status of each case’s surveillance form and Perinatal Mortality Review Tool review;
- the Trust/Health Board Reported Cases list provides abbreviated details of all deaths reported;
- the Trust/Health Board Summary provides the number of deaths by year, case-type and unit;
- the Trust/Health Board Case Review list provides the opportunity for local reporters to check the accuracy (within a fixed time frame) of the data reported by their organisation prior to the analysis for the report.
In addition, users can access a real-time data monitoring tool which allows them to view, filter and summarise live surveillance data for their Trust.
Web browser compatibility
The security requirements of the NHS in relation to electronic data flows mandate that the highest levels of security be employed. In order for this to be achieved, those accessing the MBRRACE-UK reporting system need access to an up-to-date web browser compatible with these security specifications. Appropriate browsers are available to download free of charge, although the installation of such software may require the co-operation of local NHS IT departments.
3.3. Ensuring all births and extended perinatal deaths are identified
Data sources
The sources of data used to ensure complete data collection of births and extended perinatal deaths for this cohort are listed below:
England and Wales
- Birth registration data – ONS
- Death registration data – ONS
- PDS data on all births – NHS Digital (PDS)
Scotland
- Birth registration data – NRS
- Death registration data – NRS
- Maternity Inpatient and Day Case Dataset (SMR02) inpatient data - PHS, NHS National Statistics Scotland
Northern Ireland
- Birth registration data - NIMACH, Health and Social Care Public Health Agency – derived from NIMATS
- Death registration data - NIMACH, Health and Social Care Public Health Agency – derived from NIMATS
- Inpatient data - NIMACH, Health and Social Care Public Health Agency – derived from NIMATS
Crown Dependencies
- Birth registration data - Health and Social Services Department, States of Guernsey
- Death registration data - Health and Social Services Department, States of Guernsey
- Birth registration data - Health Intelligence Unit, Public Health Services, States of Jersey
- Death registration data - Health Intelligence Unit, Public Health Services, States of Jersey
- PDS data on all births, Isle of Man – NHS Digital (PDS)
Identifying all extended perinatal deaths
Statutorily registered deaths which meet the MBRRACE-UK reporting criteria are matched to the deaths reported to MBRRACE-UK in order to identify any stillbirths or neonatal deaths which have not been reported to MBRRACE-UK. Due to the different system of implementation in Northern Ireland, the NIMACH office staff ensured full ascertainment of their data on our behalf.
For England, Wales and Scotland the matching is performed using a combination of deterministic and probabilistic matching methods based on the mother’s given name, mother’s family name, postcode of residence at time of delivery, Trust or Health Board of birth, baby’s NHS number (England – where available), CHI number (Scotland), gestational age at delivery, birthweight, date of delivery and date of death.
Once the checking is complete the MBRRACE-UK Lead Reporters are notified of any known deaths that have occurred in their Trust or Health Board which could not be identified on the MBRRACE-UK system and asked to confirm that this was a death in their organisation and provide the missing information.
This checking for deaths missing from the MBRRACE-UK database cannot start until information on statutorily registered deaths are provided to MBRRACE-UK by ONS (England and Wales) and NRS (Scotland), meaning that we cannot inform MBRRACE-UK Lead Reporters of missing deaths until some months after the event. Although most missing deaths can be identified in this way, not all deaths to be reported to MBRRACE-UK are available from statutory sources in a timely manner:
- A small percentage of statutorily registered deaths are registered only after considerable delay, most often because an inquest was being held;
- Late fetal losses delivered at 22 to 23 completed weeks’ gestational age are not officially registered;
- RCOG guidance is that stillbirths delivered at 24 completed weeks’ gestational age or greater where the death was confirmed before 24 completed weeks’ gestational age should not be registered as stillbirths; however, in order to investigate variations in the reporting of stillbirths occurring at around 24 completed weeks’ gestational age, these deaths should all be reported to MBRRACE-UK.
There are no timely and easily accessible data sources for deaths that have not been officially registered and, therefore, it is not possible to ensure that all of these deaths have been reported to MBRRACE-UK.
Identifying all births
Individual information on all births in the UK and Crown Dependencies is obtained in order to generate mortality rates adjusted for maternal, baby, and socio-demographic risk factors. Information for England, Wales and the Isle of Man (PDS and ONS birth registration data), Scotland (NRS and PHS), Northern Ireland (NIMATS), Bailiwick of Guernsey (Health and Social Services Department) and the Bailiwick of Jersey (Health Intelligence Unit) is combined to give a single dataset of births for the whole UK and Crown Dependencies. This data is then combined with the information on the deaths to obtain the final data for analysis.
The allocation of births to an organisation is complex, given the wide variation in the recording of the notifying organisation, and it is not always possible to easily identify the place of birth from the data reported. In many cases this either requires further detailed enquiry or correction of the place of birth, where an incorrect organisation has inadvertently been recorded. Complete and accurate recording is vital to enable MBRRACE-UK to allocate births to the appropriate Trust or Health Board for analysis and reporting.
Home births are allocated to the Trust or Health Board responsible for this service, whenever this is recorded, in order for the correct denominator(s) to be calculated. All Trusts and Health Boards in England, Wales and the Isle of Man completing information for the PDS should ensure that they are identified as the notifying organisation for all births related to their service.
3.4. Generating the births dataset
The births and extended perinatal deaths identified using the sources and methods described above are combined to generate a single dataset for analysis. Due to the variations in the data sources from the different countries, this is undertaken separately for each set of data sources as described below. Once the datasets have been generated for each country these are combined into a final, single dataset for analysis.
England and Wales
The complete dataset of births and extended perinatal deaths for England and Wales is generated using birth registration data (ONS), death registration data (ONS), PDS records, and MBRRACE-UK death notification records. The process undertaken by MBRRACE-UK is:
-
All datasets are restricted to births in the reported year.
-
All records of births are combined into a single dataset (Figure 1): i.e. livebirth registrations (ONS); stillbirth registrations (ONS); PDS birth records; MBRRACE-UK notifications of late fetal losses. All of these datasets are used in order to obtain complete ascertainment of all births in England and Wales:
- late fetal losses are only recorded in the MBRRACE-UK death records;
- late birth registrations are captured by the PDS records;
-
Births at less than 22 completed weeks’ gestational age and pregnancies ended by a termination of pregnancy are removed from the dataset of births, as these are not reported by MBRRACE-UK.
-
Births at 22 to 23 completed weeks’ gestational age are removed from the dataset of births for the main tables and maps as these births are currently reported separately by MBRRACE-UK.
-
All records of late fetal losses, stillbirths, and neonatal deaths are combined into a single dataset (Figure 2): i.e. death registrations (ONS); MBRRACE-UK death notifications. Both of these datasets are used in order to obtain complete ascertainment of all extended perinatal deaths in England and Wales.
-
All deaths where the births occurred at less than 22 completed weeks’ gestational age and pregnancies ended by a termination of pregnancy are removed from the dataset of deaths as these are not reported by MBRRACE-UK.
-
All deaths where the births occurred at less than 24 completed weeks’ gestational age are removed from the dataset of deaths for the main tables and maps as these deaths are currently reported separately by MBRRACE-UK.
-
The dataset of deaths are merged into the dataset of births in order to create a single dataset for analysis.
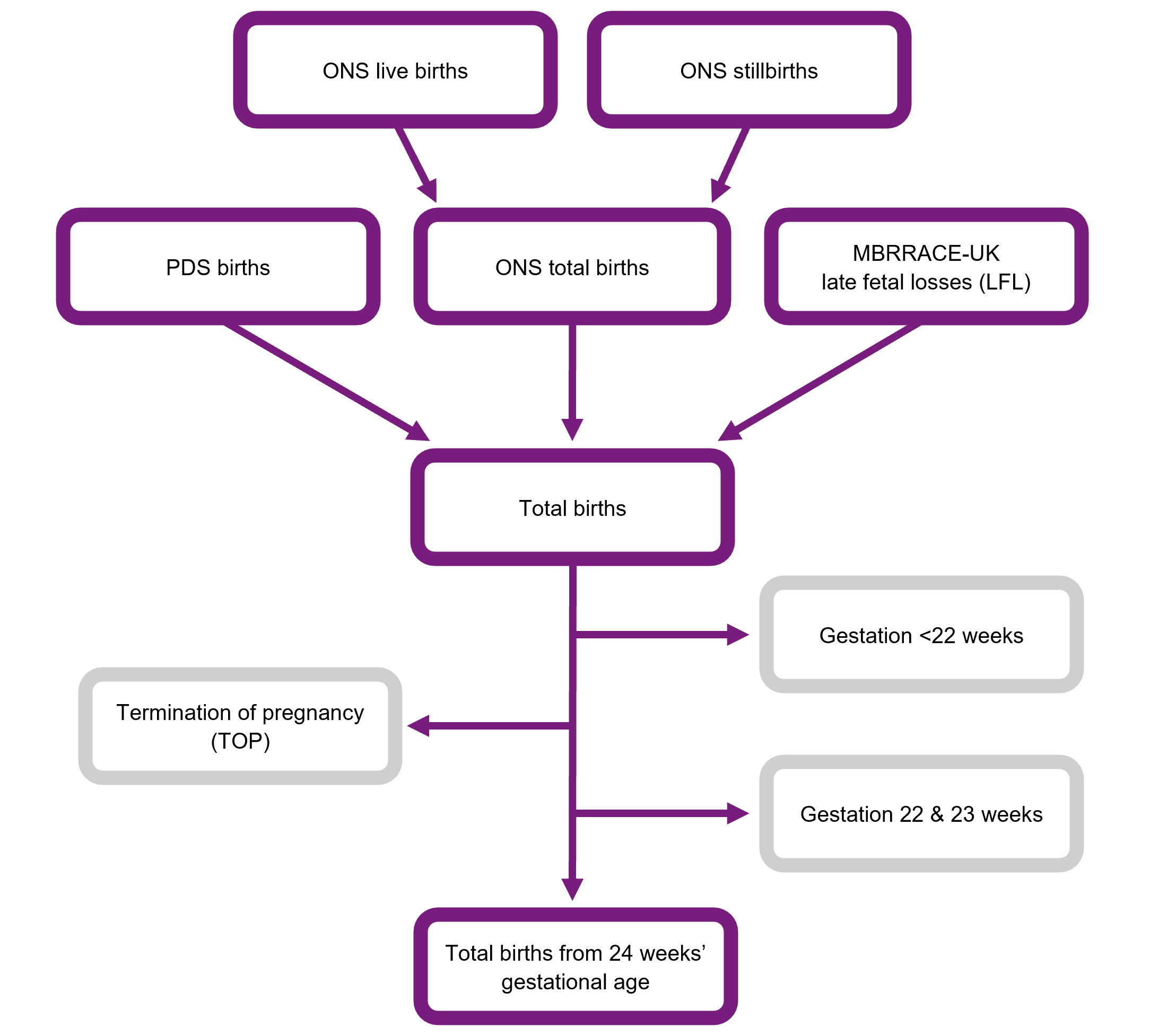
Description of Figure 1: Flow chart showing how datasets from multiple sources are combined in order to generate a complete births dataset for England and Wales.
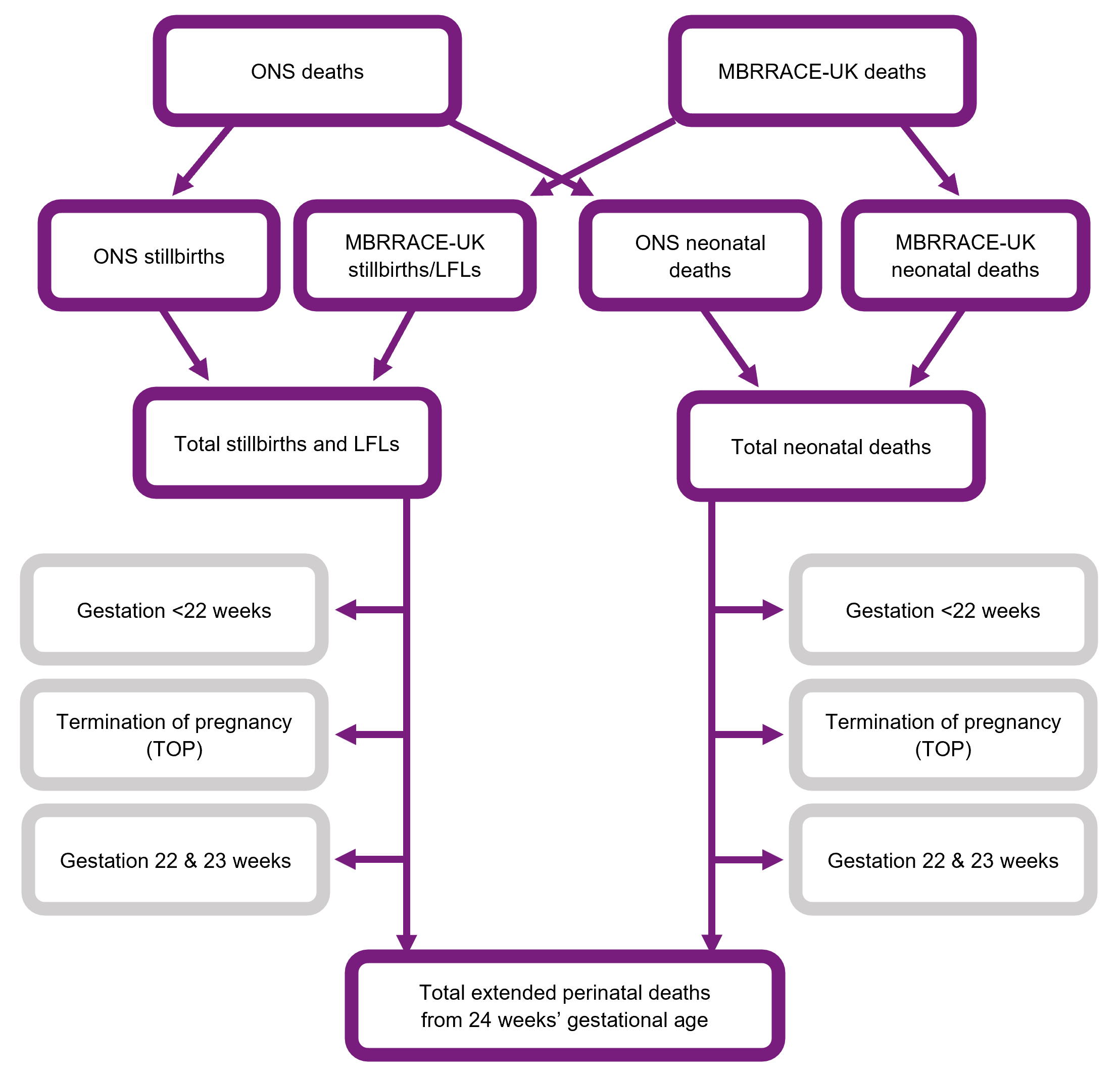
Description of Figure 2: Flow chart showing how datasets from multiple sources are combined in order to generate a complete extended perinatal deaths dataset for England and Wales.
Scotland
The complete dataset of births and extended perinatal deaths for Scotland is generated using a similar approach to that used for England and Wales. For Scotland, data is obtained from birth registration data (NRS), death registration data (NRS), SMR02 Maternity Inpatient and Day Care Case records (PHS), and MBRRACE-UK death notification records. The birth registration data and the SMR02 data are merged before being released to MBRRACE-UK (PHS). The process undertaken by MBRRACE-UK is:
Step 1: All datasets are restricted to births in the reported year.
Step 2: All records of births are combined into a single dataset (Figure 3): i.e. birth registrations/SMR02 (PHS); PHS notifications of late fetal losses; MBRRACE-UK notifications of late fetal losses. These datasets are used in order to obtain complete ascertainment of all births in Scotland.
Step 3: Births at less than 22 completed weeks’ gestational age and pregnancies ended by a termination of pregnancy are removed from the dataset of births as these are not reported by MBRRACE-UK.
Step 4: Births at 22 to 23 completed weeks’ gestational age are removed from the dataset of births for the main tables and maps as these births are currently reported separately by MBRRACE-UK.
Step 5: All records of late fetal losses, stillbirths, and neonatal deaths are combined into a single dataset (Figure 4): i.e. death registrations and SMR02 (PHS); MBRRACE-UK death notifications. Both of these datasets are used in order to obtain complete ascertainment of all extended perinatal deaths in Scotland.
Step 6: All deaths where the births occurred at less than 22 completed weeks’ gestational age and pregnancies ended by a termination of pregnancy are removed from the dataset of deaths as these are not reported by MBRRACE-UK.
Step 7: All deaths where the births occurred at less than 24 completed weeks’ gestational age are removed from the dataset of deaths for the main analyses, as these deaths are currently reported separately by MBRRACE-UK.
Step 8: The dataset of deaths is merged into the dataset of births in order to create a single dataset for analysis.
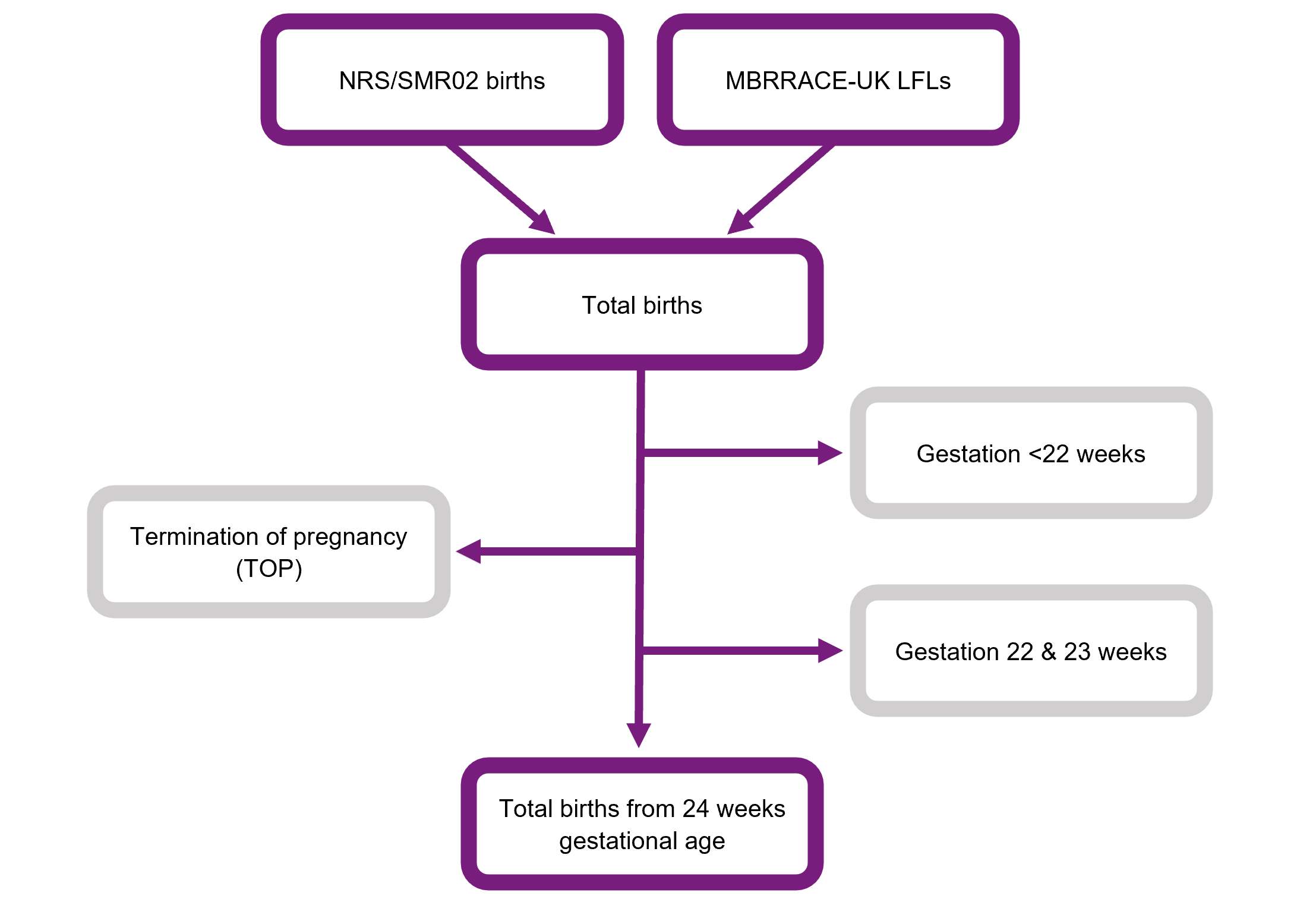
Description of Figure 3: Flow chart showing how datasets from multiple sources are combined in order to generate a complete births dataset for Scotland.
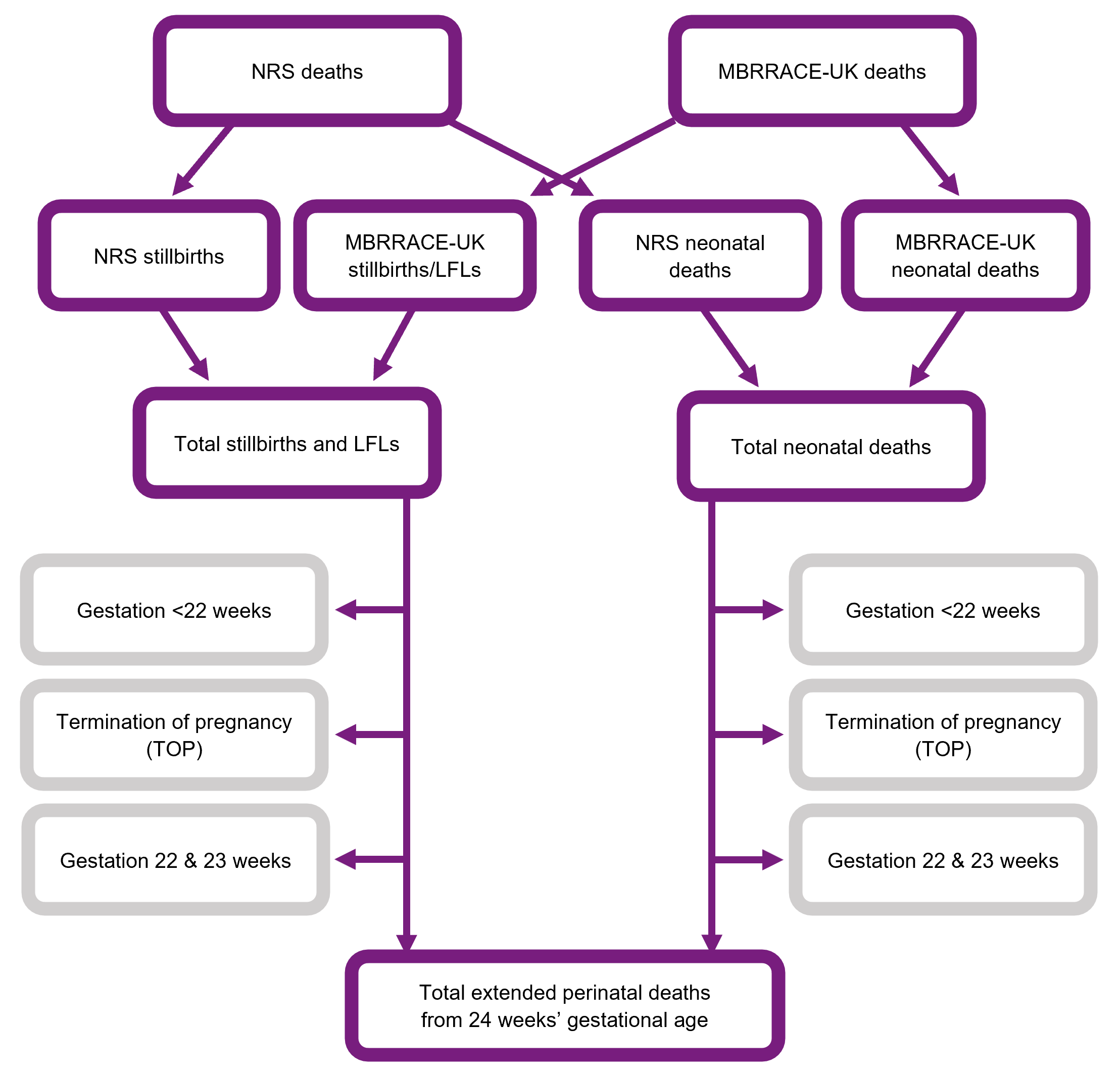
Description of Figure 4: Flow chart showing how datasets from multiple sources are combined in order to generate a complete extended perinatal deaths dataset for Scotland.
Northern Ireland and the Crown Dependencies
Datasets of births and extended perinatal deaths for Northern Ireland, the Bailiwick of Guernsey and the Bailiwick for Jersey are supplied to MBRRACE-UK as complete datasets from the appropriate national data providers. The birth records for the Isle of Man are obtained from the PDS records. In each case the birth and death records are then linked to the MBRRACE-UK records.
Data cleaning, linking and derived variables
Where information on a variable is available from more than one source a ‘best value’ algorithm is applied in order to obtain the value to be included in the analyses. The algorithm chosen is:
- where available, the value recorded in the MBRRACE-UK death record is used as the prime source;
- if unavailable (e.g. the baby survived the neonatal period) the value recorded in the statutory birth or death registration record is taken as the secondary source;
- for England and Wales, the value recorded in the PDS record is used as the third source: the gestational age at delivery is only available from the PDS records.
3.5. Location of mother’s residence
The postcode of the mother’s residence at the time of delivery is used to identify the country, ICB (England), Health Board (Scotland and Wales), Health and Social Care Trust (Northern Ireland), Crown Dependency, and Local Authority of reporting using postcode linked data supplied as part of GridLink. In addition, it is used to obtain the appropriate value for the child poverty index.
The Trust or Health Board of birth is derived using the most appropriate source from all available datasets. For England and Wales the recorded Communal Establishment Code in the ONS birth records is used as the primary source the location of the birth. When the place of birth cannot not be located from the ONS records (e.g. births at home and in-transit) the location is derived from the PDS record. If neither record provided a clear Trust or Health Board of birth then an estimate is made based on the postcode of birth.
The Trust or Health Board of death is obtained directly from the MBRRACE-UK death record.
4. Data items reported to MBRRACE-UK
Download as MS Excel spreadsheet5. Definitions and abbreviations
5.1 Definitions used by MBRRACE-UK
| Late fetal loss | A baby delivered between 22 and 23 completed weeks’ gestational age showing no signs of life, irrespective of when the death occurred. |
| Stillbirth | A baby delivered at or after 24 completed weeks’ gestational age showing no signs of life, irrespective of when the death occurred. |
| Antepartum stillbirth | A baby delivered at or after 24 completed weeks’ gestational age showing no signs of life and known to have died before the onset of care in labour. |
| Intrapartum stillbirth | A baby delivered at or after 24 completed weeks’ gestational age showing no signs of life and known to have been alive at the onset of care in labour. |
| Neonatal death | A liveborn baby (born at 20 completed weeks’ gestational age or later, or with a birthweight of 400g or more where an accurate estimate of gestation is not available), who died before 28 completed days after birth. |
| Early neonatal death | A liveborn baby (born at 20 completed weeks’ gestational age or later, or with a birthweight of 400g or more where an accurate estimate of gestation is not available) who died before 7 completed days after birth. |
| Late neonatal death | A liveborn baby (born at 20 completed weeks’ gestational age or later, or with a birthweight of 400g or more where an accurate estimate of gestation is not available) who died after 7 completed days but before 28 completed days after birth. |
| Perinatal death | A stillbirth or early neonatal death. |
| Extended perinatal death | A stillbirth or neonatal death. |
| Termination of pregnancy | The deliberate ending of a pregnancy, normally carried out before the embryo or fetus is capable of independent life. |
5.2. Abbreviations
| BMI | Body Mass Index |
| CHI | Community Health Index (Scotland) |
| CI | Confidence Interval |
| CODAC | Cause Of Death & Associated Conditions |
| EDD | Estimated Date of Delivery |
| HQIP | Healthcare Quality Improvement Partnership |
| ICB | Integrated Care Board |
| ICS | Integrated Care System |
| LFL | Late Fetal Loss |
| MBRRACE-UK | Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK |
| MNI-CORP | Maternal, Newborn and Infant Clinical Outcome Review Programme |
| NICU | Neonatal Intensive Care Unit |
| NIMACH | Northern Ireland Maternal and Child Health |
| NIMATS | Northern Ireland Maternity System |
| NISRA | Northern Ireland Statistics and Research Agency |
| NRS | National Records of Scotland |
| ONS | Office for National Statistics |
| PDS | Personal Demographics Service |
| PHS | Public Health Scotland |
| PMRT | Perinatal Mortality Review Tool |
| RCOG | Royal College of Obstetricians and Gynaecologists |
| SMR | Standardised Mortality Ratio |
| SMR02 | Maternity Inpatient and Day Case Dataset (Scotland) |
6. Additional information
6.1. Funding
The Maternal, Newborn and Infant Clinical Outcome Review Programme, delivered by MBRRACE-UK, is commissioned by the Healthcare Quality Improvement Partnership (HQIP) as part of the National Clinical Audit and Patient Outcomes Programme (NCAPOP). HQIP is led by a consortium of the Academy of Medical Royal Colleges, the Royal College of Nursing, and National Voices. Its aim is to promote quality improvement in patient outcomes. The Clinical Outcome Review Programmes, which encompass confidential enquiries, are designed to help assess the quality of healthcare, and stimulate improvement in safety and effectiveness by systematically enabling clinicians, managers, and policy makers to learn from adverse events and other relevant data. HQIP holds the contract to commission, manage, and develop the National Clinical Audit and Patient Outcomes Programme (NCAPOP), comprising around 40 projects covering care provided to people with a wide range of medical, surgical and mental health conditions. The programme is funded by NHS England, the Welsh Government and, with some individual projects, other devolved administrations and Crown Dependencies.
More details can be found on the HQIP website.
6.2. Stakeholder involvement
Organisations representing parents and families are involved in the MBRRACE-UK programme as part of the ‘Third Sector’ stakeholder group, identifying possible areas for future research and helping to communicate key findings and messages from the programme to parents, families, the public and policy makers, including through the development of lay summary reports. A full list of organisations can be found in the acknowledgements.
6.3. Attribution
This manual should be cited as:
Draper ES, Gallimore ID, Smith LK, Matthews RJ, Fenton AC, Kurinczuk JJ, Smith PW, Manktelow BN, on behalf of the MBRRACE-UK Collaboration. MBRRACE-UK Perinatal Mortality Surveillance: Technical Manual. Leicester: The Infant Mortality and Morbidity Studies, Department of Population Health Sciences, University of Leicester. 2023.
Published by:
The Infant Mortality and Morbidity Studies
Department of Population Health Sciences
University of Leicester
George Davies Centre
University Road
Leicester LE1 7RH
7. Version history
| Version | Details of changes | Release date |
|---|---|---|
| 1.0. | First release | 10/12/2020 |
| 1.1. | Data sources for Scotland updated | 14/10/2021 |
| 1.2. | Section 3.2. "The system for online data submission" updated | 14/09/2023 |
| 1.3. | Section 2. "Statistical methods" updated. Sections 2.1. and 2.2. simplified. | 20/02/2024 |
| 1.4. | Section 2.3. "Risk-adjustment factors" updated. Link to revised child poverty measures added. | 05/02/2025 |