MBRRACE-UK perinatal mortality surveillance
UK perinatal deaths of babies born in 2023
State of the nation report
Contents
1. Introduction
1.1. Report overview
This is the eleventh MBRRACE-UK Perinatal Mortality Surveillance Report. The report is divided into five sections: perinatal mortality rates in the UK; mortality rates for Trusts and Health Boards; mortality rates by gestational age; mortality rates by ethnicity and socio-economic deprivation; and a description of the causes of perinatal death.
This report focuses on births from 24 completed weeks’ gestational age, with the exception of the section on mortality rates by gestational age, which also includes information on births at 22 to 23 completed weeks’ gestational age. This avoids the influence of the wide disparity in the classification of babies born before 24 completed weeks’ gestational age as a neonatal death or a late fetal loss. Terminations of pregnancy have been excluded from the mortality rates reported.
Additional supporting materials to accompany this report include:
- a set of reference tables;
- a data viewer with interactive mapping, which presents mortality rates for individual organisations, including Trusts and Health Boards; and
- a technical manual containing full details of the MBRRACE-UK methodology, including definitions, case ascertainment and statistical methods.
A summary version of the report is available to download as a PDF. You can also download a Plain English summary of the key findings, which explains the main points of the report in clear, straightforward language.
1.2. Definitions and terminology
For definitions of the deaths reported to MBRRACE-UK and an explanation of the different types of mortality rates reported, see the MBRRACE-UK technical manual.
In this report we use the terms ‘women’ and ‘mothers’. However, we acknowledge that not all people who access perinatal services identify as women, and that our recommendations apply to all people who are pregnant or have given birth. Likewise, use of the word ‘parents’ includes anyone who has the main responsibility of caring for a baby.
2. Perinatal mortality rates in the UK: 2023
2.1. Introduction
Rates of stillbirth, neonatal mortality and extended perinatal mortality are presented by country of residence for the UK and for each devolved nation for the period 2013 to 2023. This is to show trends in mortality rates over time and to enable individual nations to monitor the progress of initiatives to reduce perinatal mortality,
2.2. Key messages
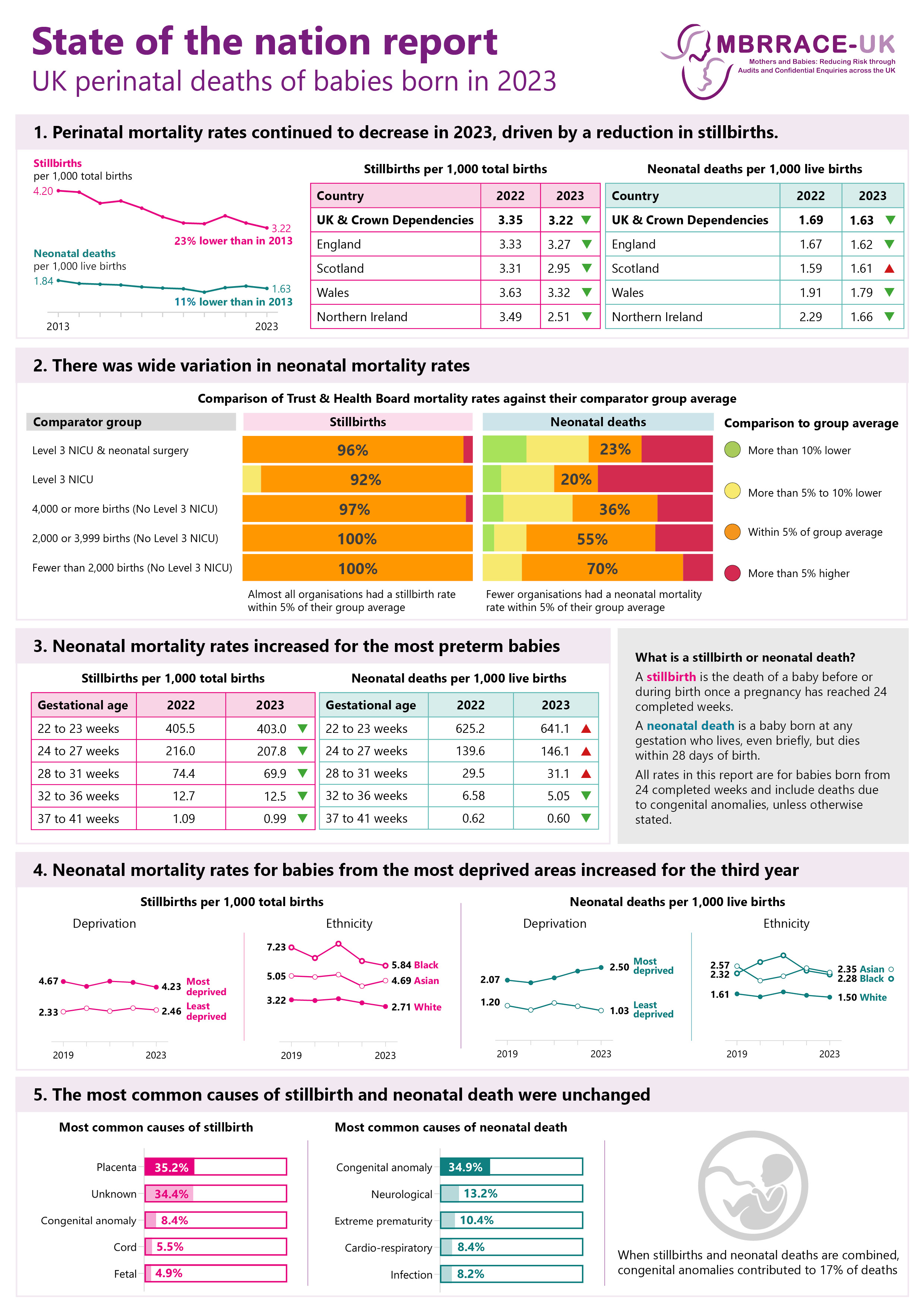
- Extended perinatal mortality rates decreased across the UK in 2023 (UK extended perinatal mortality rate: 4.84 per 1,000 total births). The long-term reduction in perinatal mortality is driven largely by a reduction in stillbirths.
- Compared with rates in 2022, stillbirth rates per 1,000 total births in 2023 were lower across the UK: 3.22 (UK); 3.27 (England); 2.95 (Scotland); 3.32 (Wales); and 2.51 (Northern Ireland).
- There were decreases in the neonatal mortality rate per 1,000 live births in England, Wales and Northern Ireland compared with 2022: 1.63 (UK); 1.62 (England); 1.61 (Scotland); 1.79 (Wales); and 1.66 (Northern Ireland).
2.3. Perinatal mortality rates across the UK
Data sources: MBRRACE-UK, PDS, ONS, NRS, PHS, NIMATS, States of Guernsey, States of Jersey.
Description of Figure 1: Line charts showing stillbirth (all, antepartum and intrapartum), neonatal death (all, early and late)and extended perinatal mortality rates for the UK, England, Scotland, Wales and Northern Ireland, from 2013 to 2023. Stillbirths and extended perinatal deaths are shown as rates per 1,000 total births. Neonatal deaths are shown as rates per 1,000 live births. Births at less than 24 completed weeks’ gestational age and terminations of pregnancy are excluded.
2.4. Births and perinatal deaths
In 2023, there were 661,008 total births at 24 completed weeks or greater gestational age (excluding terminations of pregnancy) in the UK. This was a decrease of 14,883 births (2.3%) compared with 675,891 in 2022. Since the start of the MBRRACE-UK programme in 2013, births have fallen by 120,924 (18.3%).
There were 2,128 stillbirths and 1,074 neonatal deaths in 2023. This was 1,158 (35.2%) fewer stillbirths and 362 (25.2%) fewer neonatal deaths compared with 2013.
3. Perinatal mortality rates for Trusts and Health Boards
3.1. Introduction
To account for the wide variation in case-mix, Trusts and Health Boards were classified hierarchically into five mutually exclusive comparator groups, based on their level of service provision. In order to compare Trusts and Health Boards more fairly, stabilised & adjusted mortality rates were calculated and colour-coded according to the variation from their respective comparator group average. A complete explanation of the MBRRACE-UK methodology, including statistical methods, can be found in the technical manual.
Where there is only a small number of births in an organisation it is difficult in any one year to be sure that any extreme value seen for the crude mortality rate is real and not just a chance finding. A stabilised rate allows for the effects of chance variation due to small numbers. The mortality rates are also adjusted to account for key factors which are known to increase the risk of perinatal mortality. The extent of the adjustment is limited to those factors that are collected for all births across the whole of the UK: mother’s age; socio-economic deprivation based on the mother’s residence; baby’s ethnicity; baby’s sex; whether they are from a multiple birth; and gestational age at birth (neonatal deaths only). A complete explanation of the MBRRACE-UK methodology, including statistical methods, can be found in the technical manual.
3.2. Key messages
- Stabilised & adjusted stillbirth rates in 2023 continued to show limited variation, with 97.4% of Trusts and Health Boards having a stabilised & adjusted stillbirth rate within 5% of their comparator group average.
- For stabilised & adjusted neonatal mortality, rates showed wider variation, with 41.7% of Trusts and Health Boards being within 5% of their comparator group average.
- After the exclusion of deaths due to congenital anomalies, 52.3% of Trusts and Health Boards had a stabilised & adjusted neonatal mortality rate within 5% of their comparator group average.
3.3. Variation in perinatal mortality rates within Trust and Health Board comparator groups
Data sources: MBRRACE-UK, PDS, ONS, NRS, PHS, NIMATS, States of Guernsey, States of Jersey.
Description of Figure 2: Scatter chart showing the variation in stabilised & adjusted stillbirth, neonatal death and extended perinatal mortality rates within Trust and Health Board comparator groups in 2023. Trusts and Health Boards are grouped according to their level of service provision, with dots representing individual Trusts and Health Boards and a vertical line representing the comparator group average. Extended perinatal deaths are also shown without deaths due to congenital anomalies. Stillbirths and extended perinatal mortality rates are shown as rates per 1,000 total births. Neonatal mortality rates are shown as rates per 1,000 live births. Births at less than 24 completed weeks’ gestational age and terminations of pregnancy are excluded.
3.4. The effect of congenital anomalies on perinatal mortality rates
Deaths due to congenital anomalies continue to account for a large proportion of perinatal deaths (see Section 6). When deaths due to congenital anomalies were excluded, variation in stabilised & adjusted stillbirth rates compared to the comparator group average increased, with 68.2% of Trusts and Health Boards falling within 5% of the group average.
Exclusion of deaths due to congenital anomalies reduced the variation in stabilised & adjusted neonatal mortality rates, with 52.3% of Trusts and Health Boards having a rate within 5% of their comparator group average. However, within the comparator group most likely to care for these babies (Level 3 NICU and neonatal surgery), only 38.5% of Trusts and Health Boards were within 5% of the group average.
3.5. Mortality rates for Trusts and Health Boards
Mortality rates for individual Trusts and Health Boards, including comparison to their respective comparator group average, can be found in the data viewer. The viewer also contains details of mortality rates for other organisations responsible for providing or commissioning perinatal services.
3.6. Additional data on maternity and neonatal services
Detailed data on the care provided by maternity and neonatal services is available from the National Maternity & Perinatal Audit (NMPA) and the National Neonatal Audit Programme (NNAP). The NMPA measures various aspects of maternity and neonatal care provided by NHS maternity services in England, Scotland and Wales. The NNAP assesses whether babies admitted to neonatal units in England, Scotland, Wales and the Isle of Man receive consistent high quality care.
4. Mortality rates by gestational age
4.1. Introduction
Mortality rates by gestational age group are presented to monitor the progress of national initiatives to reduce preterm births.
4.2. Key messages
- Late fetal loss and stillbirth rates decreased in 2023 across all gestational age groups compared to 2022, with the largest reduction being for babies born at 37 to 41 completed weeks.
- Neonatal mortality increased in 2023 for babies born between 24 and 31 completed weeks compared to 2022. For babies born at 32 weeks or later, neonatal mortality decreased compared to 2022.
- The proportion of neonatal deaths among babies born at 22 to 23 completed weeks continued to rise, accounting for 25.1% of all neonatal deaths.
- 76.1% of stillbirths and late fetal losses and 74.5% of neonatal deaths were born preterm (before 37 completed weeks).
4.3. Late fetal loss, stillbirth and neonatal mortality rates by gestational age
Stillbirths (includes late fetal losses)
Neonatal deaths
Data sources: MBRRACE-UK, PDS, ONS, NRS, PHS, NIMATS, States of Guernsey, States of Jersey.
Description of Figure 3: Combined line and bar charts showing rates and proportions of stillbirths and neonatal deaths for babies born in the UK from 2019 to 2023, by gestational age group in completed weeks: 22 to 23, 24 to 27, 28 to 31, 32 to 36, 37 to 41. Early and late neonatal mortality rates are shown for babies born at 22 to 23 and 24 to 27 completed weeks. Deaths of babies born at 42 weeks and above are not shown due to the small numbers of births at this gestation. Stillbirths are shown as rates per 1,000 total births. Neonatal deaths are shown as rates per 1,000 live births. Terminations of pregnancy are excluded.
4.4. The impact of preterm birth
The effect of preterm birth in relation to both stillbirth and neonatal death rates in the UK remains unchanged. Despite only 8% of babies being born before 37 weeks’ gestational age, they continue to make up three-quarters of stillbirths, including late fetal losses (76%), and neonatal deaths (75%). Including babies born at 22 to 23 weeks’ gestational age, an increasing proportion of babies were born extremely preterm (less than 28 weeks’ gestational age): 38% of stillbirths and 48% of neonatal deaths.
4.5. Babies born at 42 weeks' gestational age or later
The small number of babies born at 42 weeks’ gestational age or later means that rates are subject to higher levels of yearly variation.
5. Mortality rates by socio-economic deprivation and ethnicity
5.1. Introduction
To explore inequalities in perinatal outcomes, rates of stillbirth and neonatal death are compared for area level socio-economic deprivation based on the mother’s postcode of residence at the time of the birth, and the baby’s ethnic group.
5.2. Key messages
- Despite an 8% decrease in stillbirth rates for babies born to mothers from the most deprived areas (from 4.60 per 1,000 total births in 2022 to 4.23 per 1,000 total births in 2023), the rates remain much higher than those for babies born to mothers from the least deprived areas (2.46 per 1,000 total births).
- Disparities in neonatal mortality rates by socioeconomic deprivation widened further in 2023. Rates increased for babies born to mothers from the most deprived areas (from 2.38 per 1,000 live births in 2022 to 2.50 in 2023), a rate now more than double that of babies born to mothers in the least deprived areas, where the rate decreased from 1.18 per 1,000 live births in 2022 to 1.03 in 2023.
- Stillbirth rates by ethnicity decreased in 2023 for babies of Black and White ethnicity, but increased by 9.8% for babies of Asian ethnicity compared to 2022. Babies of Black ethnicity remain more than twice as likely to be stillborn than babies of White ethnicity (Black: 5.84 per 1,000 total births; White: 2.71 per 1,000 total births).
- Neonatal mortality rates decreased in 2023 for babies of all ethnicities compared to 2022. However, babies of both Asian and Black ethnicity continue to have much higher rates of neonatal mortality than babies of White ethnicity (Asian: 2.35 per 1,000 live births; Black: 2.28 per 1,000 live births; White: 1.50 per 1,000 live births).
5.3. Socio-economic deprivation
Data sources: MBRRACE-UK, PDS, ONS, NRS, PHS, NIMATS, States of Guernsey, States of Jersey.
Description of Figure 4: Line charts showing stillbirth and neonatal mortality rates by level of socio-economic deprivation, 2019 to 2023. Deprivation is shown by quintile, and the most deprived quintile (Q5) is compared to the least deprived quintile (Q1). Stillbirths are shown as rates per 1,000 total births. Neonatal deaths are shown as rates per 1,000 live births. Births at less than 24 completed weeks’ gestational age and terminations of pregnancy are excluded.
Socioeconomic deprivation was measured using the Children in low-income families local measure (for births until 2022) and the Children in low income families: local area statistics (for births in 2023), based on the mother’s postcode of residence at the time of birth.
5.4. Ethnicity
Data sources: MBRRACE-UK, PDS, ONS, NRS, PHS, NIMATS, States of Guernsey, States of Jersey.
Description of Figure 4: Line charts showing stillbirth and neonatal mortality rates by babies’ ethnicity, between 2019 and 2023. Stillbirths are shown as rates per 1,000 total births. Neonatal deaths are shown as rates per 1,000 live births. Births at less than 24 completed weeks’ gestational age and terminations of pregnancy are excluded.
Mortality rates using more refined ethnic categories can be found in the accompanying reference tables. As the mortality rates for some groups are based on small numbers they are not presented here.
5.5. The combined effect of deprivation and ethnicity
Stillbirths
Neonatal deaths
Data sources: MBRRACE-UK, PDS, ONS, NRS, PHS, NIMATS, States of Guernsey, States of Jersey.
Description of Figure 6: Dumbbell charts showing stillbirth and neonatal mortality rates by babies' ethnicity and level of socio-economic deprivation, for babies born in the UK between 2021 and 2023. Deprivation is shown by quintile, and the most deprived quintile is compared to the least deprived quintile. Bubble sizes are proportionate to the percentage of births to mothers living in each deprivation quintile, by ethnicity. The smallest bubble represents the smallest proportion of births. Rates for babies of Black ethnicity are aggregated due to the small number of deaths of babies of Black Caribbean and Other Black ethnicities. Stillbirths are shown as rates per 1,000 total births. Neonatal deaths are shown as rates per 1,000 live births. Births at less than 24 completed weeks’ gestational age and terminations of pregnancy are excluded.
5.6. Ethnicity and deaths due to congenital anomalies
Stillbirths
Neonatal deaths
Data sources: MBRRACE-UK, PDS, ONS, NRS, PHS, NIMATS, States of Guernsey, States of Jersey.
Description of Figure 7: Dumbbell charts showing stillbirth and neonatal mortality rates by babies’ ethnicity, with and without deaths due to congenital anomalies, in 2023. Stillbirths are shown as rates per 1,000 total births. Neonatal deaths are shown as rates per 1,000 live births. Births at less than 24 completed weeks’ gestational age and terminations of pregnancy are excluded.
6. Causes of perinatal death
6.1. Introduction
Causes of death are reported to MBRRACE-UK using the Cause of Death & Associated Conditions (CODAC) classification system. The CODAC system has a three level hierarchical tree for the coding of both the primary cause of death and any associated conditions. The CODAC level 1 and level 2 classification for all stillbirths and neonatal deaths is available in the accompanying reference tables.
6.2. Key messages
- The most common causes of stillbirth were in the placenta, congenital anomaly, cord and fetal categories. There remains a high proportion of stillbirths with an unknown cause of death (34.4%).
- The most common causes of neonatal death were in the congenital anomaly, extreme prematurity, neurological, cardio-respiratory and infection categories.
- Congenital anomalies continue to contribute significantly to mortality rates, comprising 8.4% of stillbirths and 34.9% of neonatal deaths.
6.3. Stillbirth and neonatal mortality rates by cause of death
Stillbirths
Stillbirths
Neonatal deaths
Data sources: MBRRACE-UK, PDS, ONS, NRS, PHS, NIMATS, States of Guernsey, States of Jersey.
Description of Figure 8: Combined line and bar charts showing the five highest stillbirth and neonatal mortality rates by cause of death, between 2019 and 2023. Cause of death is shown by CODAC level 1 category for stillbirths and levels 1 and 2 for neonatal deaths. Stillbirths are shown as rates per 1,000 total births. Neonatal deaths are shown as rates per 1,000 live births. Births at less than 24 completed weeks’ gestational age and terminations of pregnancy are excluded.
6.5. Post-mortem examination
Post-mortem examination (PM) was offered to parents for 99.3% of stillbirths and 86.1% of neonatal deaths. Where a PM was offered, full or limited consent was given for 45.1% of stillbirths and 27.1% of neonatal deaths. Examination by the coroner or procurator fiscal accounted for an additional 1.7% of neonatal deaths.
6.6. Placental histology
The proportion of stillbirths with a placental examination fell again in 2023, from 93.7% in 2022 to 92.0% in 2023. For neonatal deaths on day 1 of life or where the cause of death was reported as intrapartum-related, the proportion with a placental examination also fell, from 82.5% in 2022 to 78.8% in 2023.
7. Summary and recommendations
In 2023, extended perinatal mortality rates across the UK continued to decline, reaching 4.84 per 1,000 total births, primarily driven by a reduction in stillbirths. Compared to 2022, stillbirth rates fell across all UK nations, while neonatal mortality rates also declined in England, Wales, and Northern Ireland.
Stabilised and adjusted stillbirth rates showed limited variation, with 97% of Trusts and Health Boards having rates within 5% of their comparator group average. However, neonatal mortality rates demonstrated greater variation, with only 42% of Trusts and Health Boards within the same threshold. When excluding deaths due to congenital anomalies, this figure increased to 52%.
Late fetal loss and stillbirth rates decreased across all gestational ages, with the largest reduction seen in term births (37 to 41 weeks). However, neonatal mortality increased for preterm babies born between 24 and 31 weeks, while it declined for those born at 32 weeks or later. Notably, babies born at 22 to 23 weeks accounted for an increasing proportion (25%) of all neonatal deaths. Preterm births remained a significant factor, with 76% of stillbirths and 75% of neonatal deaths occurring in babies born before 37 weeks.
Socioeconomic disparities continued to be a major concern, with stillbirth rates for babies born to mothers from the most deprived areas remaining significantly higher than those from the least deprived areas, despite an 8% decline. Neonatal mortality disparities also widened, with rates increasing for the most deprived populations and decreasing for the least deprived.
Ethnic disparities in perinatal outcomes persisted. Stillbirth rates declined for Black and White babies but increased by 10% for Asian babies. Black babies remained more than twice as likely to be stillborn as White babies. Neonatal mortality rates decreased across all ethnicities but remained highest for Asian and Black babies.
The leading causes of stillbirth were placental issues, congenital anomalies, umbilical cord complications, and fetal conditions, but 34% of stillbirths had an unknown cause. Neonatal deaths were most commonly attributed to congenital anomalies, neurological issues, extreme prematurity, cardio-respiratory complications, and infections. Congenital anomalies remained a significant contributor, accounting for 8% of stillbirths and 35% of neonatal deaths.
These findings highlight continued progress in reducing perinatal mortality but underscore the need for targeted interventions to address disparities by socioeconomic status, ethnicity, and gestational age. Recent MBRRACE-UK reports have made national level recommendations in support of these aims, but focused work at local provider, network and commissioner level may be required to understand and tackle these issues in an effective manner.
| No. | Previous recommendations with continued relevance |
|---|---|
| P1. | Ensure neonatal intensive care capacity and resources reflect the increase in the numbers of babies born before 24 completed weeks’ gestational age receiving survival-focused care. |
| P2. | Support external clinical input into the rigorous review of all stillbirths and neonatal deaths across the UK, to identify learning and common themes related to clinical care and service provision, delivery and organisation. |
| P3. | Ensure healthcare providers adopt and use the BAPM Perinatal Optimisation Pathway, to improve preterm outcomes. |
| P4. | Continue to develop and implement targeted action, at national and organisational levels, to support the reduction of direct and indirect health inequalities. |
8. Further information
8.1. Supporting materials
Additional supporting materials to accompany this report include reference tables, a data viewer for viewing and and comparing perinatal mortality rates for the organisations responsible for the commissioning and provision of care, and a technical manual. You can also download a Plain English summary of the key findings, which explains the main points of the report in clear, straightforward language.
8.2. Deaths reported to MBRRACE-UK
Deaths reported to MBRRACE-UK since 1 January 2013 are:
- late fetal losses: a baby born between 22 and 23 completed weeks’ gestational age showing no signs of life, irrespective of when the death occurred;
- stillbirths: a baby born at or after 24 completed weeks’ gestational age showing no signs of life, irrespective of when the death occurred;
- neonatal deaths: a liveborn baby (born at 20 completed weeks’ gestational age or later) who died before 28 completed days after birth.
Terminations of pregnancy resulting in a registered stillbirth (from 24 completed weeks’ gestation) or neonatal death (from 20 completed weeks’ gestation) are also notified. We collect this limited information about terminations of pregnancy in order to exclude these cases from MBRRACE-UK reported statistics on perinatal mortality.
8.3. The birth cohort
In this report rates of stillbirth, neonatal death and extended perinatal death (stillbirths and neonatal deaths combined) are presented for babies born in England, Wales, Scotland, Northern Ireland, and the Crown Dependencies, for the period 1 January 2022 to 31 December 2022 inclusive; thus, neonatal deaths of babies born in December 2022 which occurred in January 2023 are included. The reporting of mortality for a birth cohort is in contrast to statutory publications, which are based on deaths occurring or registered in a calendar year. This method of reporting allows more accurate estimates of mortality rates to be produced as appropriate denominators are available. Deaths for Guernsey are not included in 2022, but appear in trend data for previous years.
8.4. Data extraction date
The data in this report was extracted from the MBRRACE-UK database on 25 November 2024. Any changes to the database made after this date are not reflected in the report or accompanying reference tables.
8.5. Data sources
The data presented in this report is derived from a number of sources in addition to the information submitted via the MBRRACE-UK web-based reporting system: ONS, PDS, NRS, PHS, NISRA, Health and Social Services Department (Bailiwick of Guernsey), and the Health Intelligence Unit (Bailiwick of Jersey). Full details of all data sources and the case ascertainment procedure can be found in the accompanying technical manual.
8.6. Why do MBRRACE-UK statistics on stillbirths and neonatal deaths for England and Wales differ from those published by ONS?
MBRRACE-UK report on perinatal mortality for the whole of the UK and Crown Dependencies, as well as for each individual nation. The Office for National Statistics (ONS) also publishes annual data on perinatal mortality in England and Wales. ONS figures on perinatal mortality are based on all births and deaths registered via the General Register Office. This includes all stillbirths registered at 24 weeks or more gestation, in line with the Stillbirth (Definition) Act 1992, and neonatal deaths of babies born at any gestational age. Our goal is to publish data on perinatal deaths that are clinically comparable across different organisations, such as healthcare providers or the devolved nations within the UK. Since registered stillbirths and neonatal deaths are affected by some inconsistencies in reporting between organisations, we apply a rigorous definition of deaths to ensure comparability.
There are five key differences in the way MBRRACE-UK and ONS report stillbirths and neonatal deaths:
- We report stillbirths where the birth occurred from 24 completed weeks’, irrespective of when the baby died in utero (including some unregistered deaths), while ONS statistics are based only on registered stillbirths.
- We report neonatal deaths from 24 completed weeks’ gestational age. ONS has no gestational age limit.
- We don’t include deaths following termination of pregnancy, which are included in ONS figures.
- We report deaths by the year of the baby’s birth, while ONS report deaths by the year of the baby’s death.
- We report some rates by place of baby’s birth, and others by place of residence. ONS report deaths by place of residence.
Alongside this summary, we also provide a more detailed explanation of the reasons behind these differences, and their effect on the statistics we publish.
8.7. Funding
The Maternal, Newborn and Infant Clinical Outcome Review Programme, delivered by MBRRACE-UK, is commissioned by the Healthcare Quality Improvement Partnership (HQIP) as part of the National Clinical Audit and Patient Outcomes Programme (NCAPOP). HQIP is led by a consortium of the Academy of Medical Royal Colleges and the Royal College of Nursing. Its aim is to promote quality improvement in patient outcomes. HQIP holds the contract to commission, manage, and develop the National Clinical Audit and Patient Outcomes Programme (NCAPOP), comprising around 40 projects covering care provided to people with a wide range of medical, surgical and mental health conditions. The Clinical Outcome Review Programmes, which encompass confidential enquiries, are designed to help assess the quality of healthcare, and stimulate improvement in safety and effectiveness by systematically enabling clinicians, managers, and policy makers to learn from adverse events and other relevant data. The Maternal, Newborn and Infant Clinical Outcome Review Programme is funded by NHS England and the Governments of Scotland, Wales, Northern Ireland, Jersey, Guernsey and the Isle of Man.
More details can be found on the HQIP website.
8.8. Stakeholder involvement
Organisations representing parents and families are involved in the MBRRACE-UK programme as part of the ‘Third Sector’ stakeholder group, identifying possible areas for future research and helping to communicate key findings and messages from the programme to parents, families, the public and policy makers, including through the development of lay summary reports. A full list of organisations can be found in the acknowledgements.
8.9. Attribution
This report should be cited as:
Gallimore ID, Matthews RJ, Page GL, Smith LK, Fenton AC, Knight M, Smith PW, Redpath S, Manktelow BN, on behalf of the MBRRACE-UK Collaboration. MBRRACE-UK Perinatal Mortality Surveillance, UK Perinatal Deaths of Babies Born in 2023: State of the Nation Report. Leicester: TIMMS, Department of Population Health Sciences, University of Leicester. 2025.
Published by:
TIMMS
Department of Population Health Sciences
University of Leicester
George Davies Centre
University Road
Leicester LE1 7RH
9. Version history
| Version | Details of changes | Release date |
|---|---|---|
| 1.0. | First published. | 8 May 2025 |
| 1.1. | Section 3.2. update with key messages from 2023. Figure 2 title year corrected. | 11 July 2025 |